
Breast reconstruction is one of the most challenging and rewarding areas of plastic surgery. Dr. Kind and Dr. Chang perform all types of breast reconstruction, including implant reconstruction in a single stage (“Direct to Implant”), Alloderm-assisted breast reconstruction, and microsurgical breast reconstruction. Dr. Kind and Dr. Chang are two of the very few surgeons performing the deep inferior epigastric perforator or DIEP flap for breast reconstruction. This technique allows for the breast to be reconstructed with the patient’s own tissues, without the loss of any muscle. Dr. Kind has been performing this procedure since 1998. Prior to joining Dr. Kind in 2009, Dr. Chang performed DIEP flaps at UCSF for several years. Together, they peform over 100 flaps each year. Patients from all over Northern California and beyond have come to San Francisco to be treated by Dr. Kind and Dr. Chang.
If you would like to speak to or contact one of our breast reconstruction (DIEP or implant reconstruction) patients, please contact our office.
Breast Reconstruction Overview
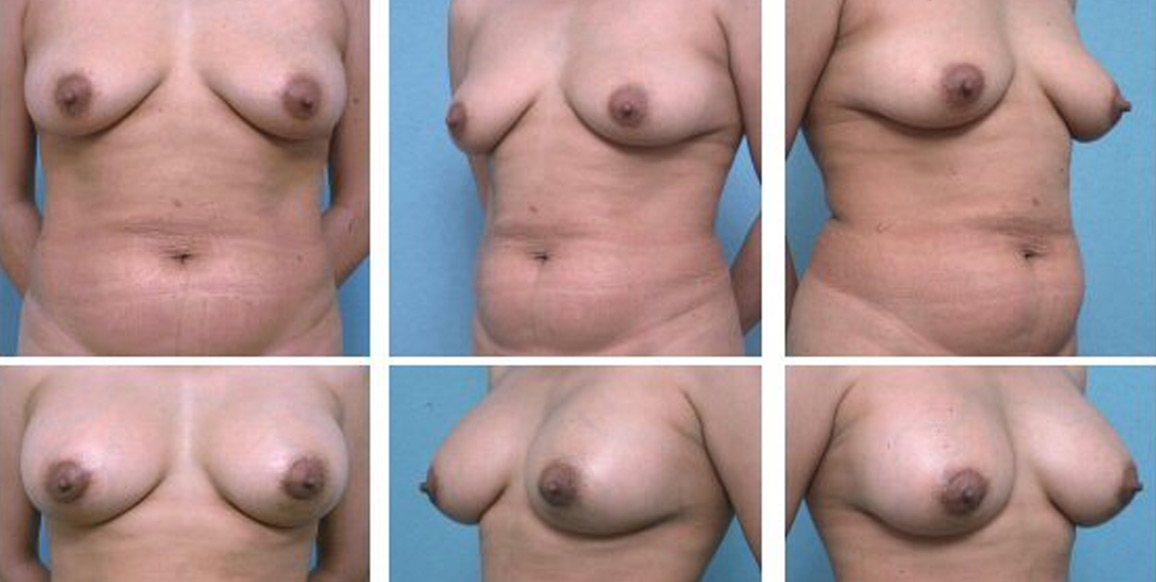
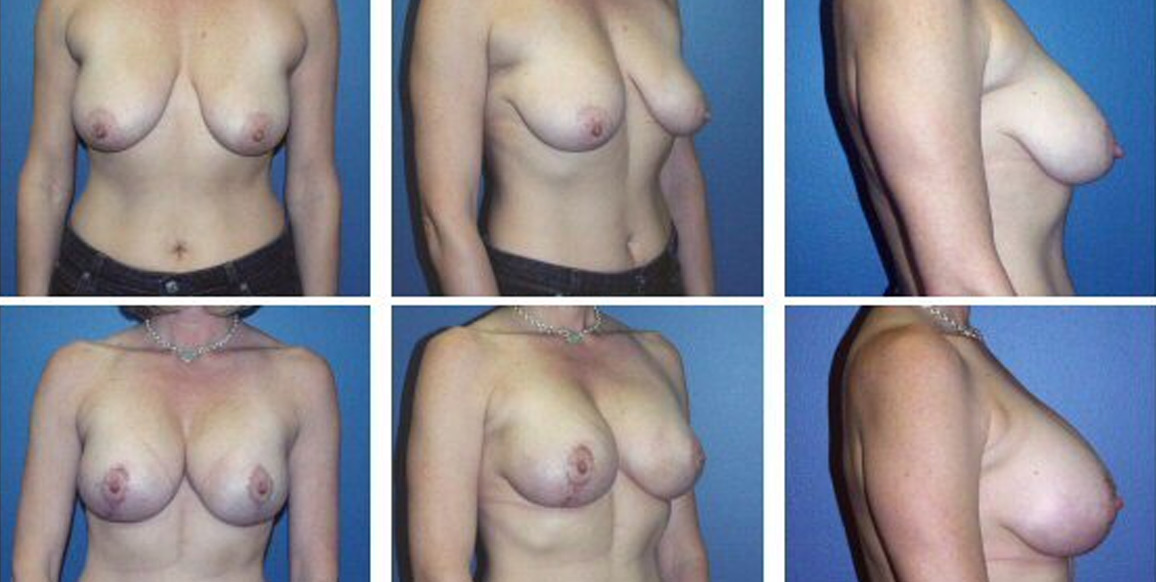
The unique circumstances of each patient help to determine the best option for the method of reconstruction that can be used. The goals of breast reconstruction surgery are to re-create a breast which matches the opposite breast, or in bilateral cases, to reconstruct two breasts of a patients’s desired size. The nipple and areola (the pigmented area surrounding the nipple) are also reconstructed. It is ideal to consult with a plastic surgeon prior to mastectomy. This allows the surgical teams to plan the treatment that is best suited for the patient, even if the patient decides to wait to have reconstructive surgery at a later date.
Immediate breast reconstruction occurs when reconstruction is performed at the time of mastectomy. Immediate reconstruction has the advantage of usually saving the patient at least one subsequent operation, and has been shown to have a significant psychological benefit, as the patient never has to experience the total loss of a breast. All of the reconstruction options listed below can be performed at the time of mastectomy.
Delayed breast reconstruction is done at a later time. For some women, this may be advised, especially if radiation to the chest area is needed after the mastectomy. Delayed reconstruction is appropriate for these women because radiation therapy following breast reconstruction can increase complications after reconstructive surgery.
There are two major types of breast reconstruction:
In this type of reconstruction a breast implant is placed in a pocket created on the chest wall. Usually this requires tissue expansion. In this process a tissue expander is filled with saline over several weeks. The patient’s body responds by stretching and creating new skin. Once the desired size of the pocket is created, a second operation is performed in which the tissue expander is removed, and a permanent implant is placed. The implants can be filled with either saline or silicone gel. Some patients can undergo breast reconstruction in a single stage. This is sometimes called “Direct to Implant” breast reconstruction. Ask your plastic surgeon if you are a candidate for this type of reconstruction.
Another option that avoids the use of tissue expansion is to cover an implant with the latissimus dorsi muscle. The latissimus dorsi is a large fan-shaped muscle of the back that can be rotated to the chest. Skin from the back can also be taken with the muscle if needed. More recently, foreign materials such as Alloderm (human cadaver allograft) have been used to create a sling to cover the lower portion of the tissue expander pocket. This can shorten the time needed for expansion, and in some cases, can allow for single-stage breast reconstruction, without the use of the latissimus dorsi muscle.
Implant reconstruction procedures have the advantage of being shorter operations, with shorter hospital stay. Generally, a fairly rapid recovery can be expected.

Autogenous Reconstruction
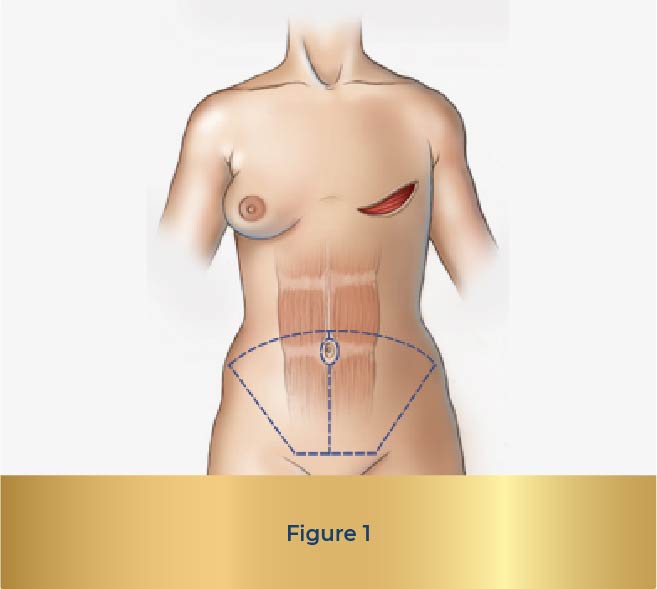
Autogenous means “one’s own”. In autogenous reconstruction, the patient’s own tissue is used to create a breast. When tissue (not just skin) is moved from one part of the body to another it is called a “flap”. There are several different flaps that are used for breast reconstruction. The most commonly performed is a “TRAM” flap. “TRAM” is an acronym for “transverse rectus abdominis myocutaneous”. This refers to the transverse (or sideways) orientation of the skin and fat taken from the lower abdomen, supplied by blood vessels that come through the rectus abdominis muscle (see figure 1). A “pedicled” TRAM flap is when the skin and fat of the lower abdomen is elevated with the underlying rectus abdominis muscle, and transferred to the chest. The skin and fat are supplied by the “pedicle” of muscle, which carries and protects the blood vessels.
The TRAM flap has many advantages. The use of the skin and fat of the lower abdomen is similar to an abdominoplasty (“tummy tuck”). Most patients are pleased to have this tissue removed. A major benefit of the TRAM, and all types of autogenous breast reconstruction, is that such reconstruction avoids the disadvantages of implant reconstruction. Breasts that are reconstructed with the patient’s own tissues usually look and feel more natural, and act more like a normal breast over time.
The main disadvantages of the TRAM flap is that compared to implant reconstruction it is a longer operation, usually requiring a longer hospital stay. In addition the TRAM flap requires the sacrifice of part or all of the rectus abdominis muscle. Most patients have minimal side effects from the loss of this muscle, although occasionally it can result in abdominal weakness, bulging, or (rarely) hernia.
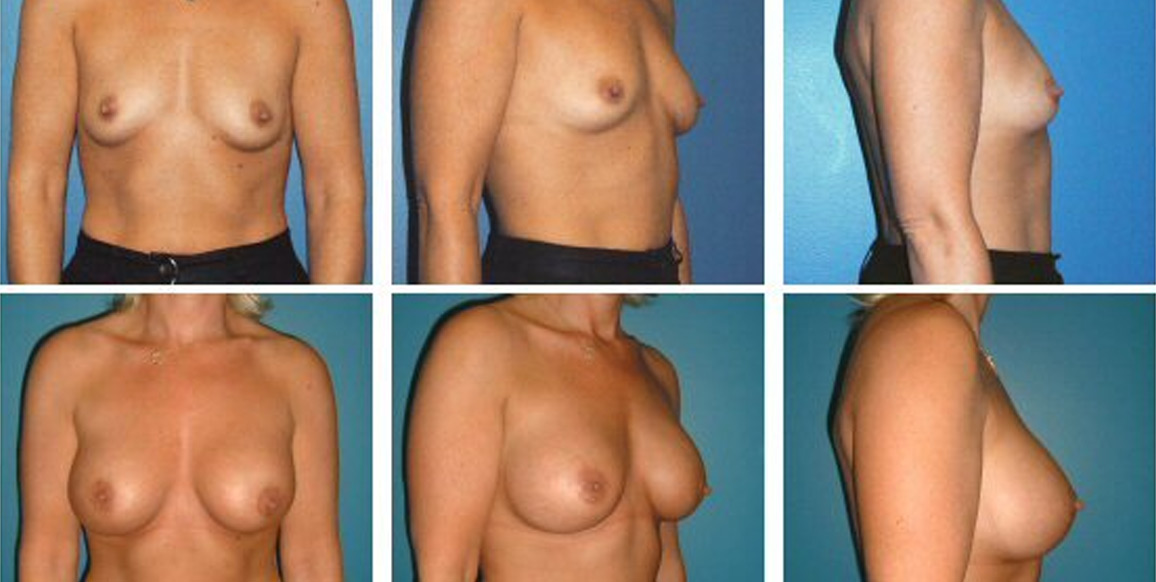
Microsurgical Reconstruction
When the TRAM flap was introduced in the early 1980’s it was recognized that the rectus abdominis muscle had blood vessels entering from both its upper and lower ends. This allowed the TRAM flap to be used as a “free” flap: the flap could be completely detached in the lower abdomen and brought to the chest, where the blood supply could be restored using microsurgical techniques
The “free” TRAM has the advantage of a more direct blood supply, so more tissue can be safely transferred. In addition, only a part of the muscle is used, which results in less damage to the abdominal wall, and a faster return to normal activities. The major disadvantage of the free TRAM is that it requires the use of microsurgical technique. Not all plastic surgeons are trained in microsurgery, and many who are prefer not to perform microsurgical breast reconstruction, because of the added complexity and the possibility of microsurgical complications. Microsurgical breast reconstruction requires the repair of small blood vessels. If the repair fails, the entire flap can be lost. Although many precautions are taken to avoid this complication, in most large series reported in the medical literature, there is a reported risk of 2 to 5%. Fortunately with the use of the implantable Doppler probe and other techniques this risk is less than 1%.
There are other types of flaps that have been introduced for microsurgical breast reconstruction, although until recently these have been performed much less commonly. Gluteal flaps are flaps taken from the buttock area, supplied by the superior or inferior gluteal artery. These flaps are most commonly used for patients who have had previous abdominal surgery, or who have minimal abdominal fat, precluding the use of the TRAM flap. The major disadvantage is that the patient must be re-positioned during the surgery, adding to the length and possible complications of the case. In addition the defect created at the donor site can be unsightly. Occasionally a patient who needs breast reconstruction will have excess tissue of the outer or inner thigh. Microsurgical flaps (tensor fascia lata, gracilis myocutaneous) from these locations can be used for breast reconstruction. In most people there is insufficient tissue to create a breast, and the donor defect created at the lateral thigh can again be problematic.



An exciting development in microsurgical reconstruction is the increasing use of perforator flaps. These flaps preserve the underlying muscle by dissecting the blood vessels through or around the muscle. Theoretically any muscle flap that includes a paddle of skin can be harvested as a perforator flap. In practice there are several perforator flaps which have been used for various reconstructive needs around the body. A few of these include the lateral arm, the anterolateral thigh, and the thoracodorsal artery perforator flaps. These flaps generally provide good thin soft tissue coverage, and since they do not include muscle, the donor defect created results in minimal deformity and less pain than a muscle flap.
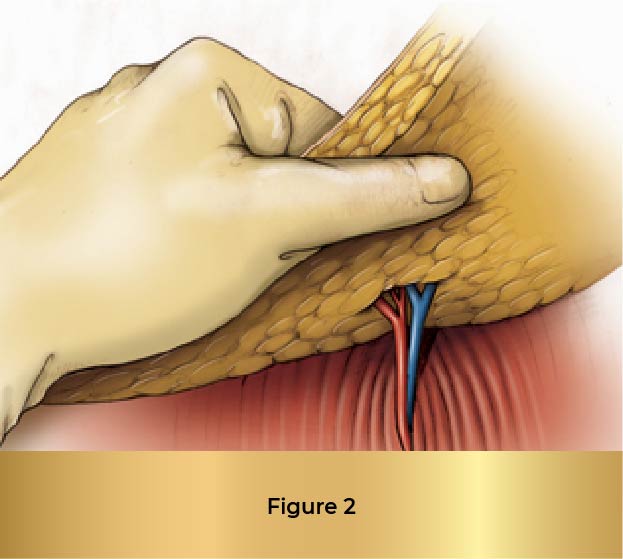
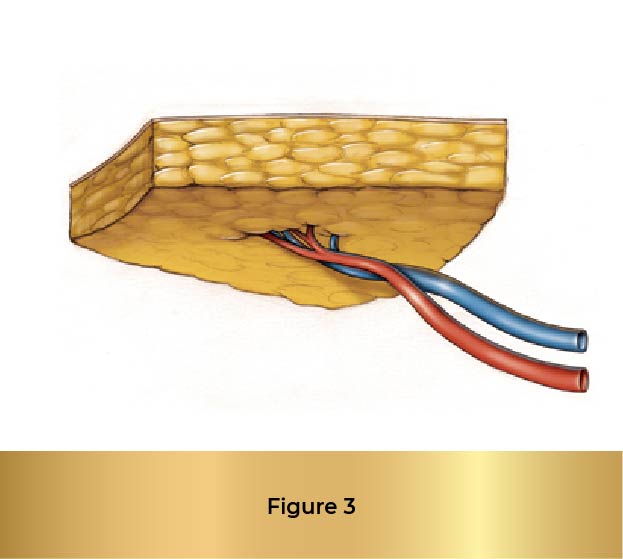
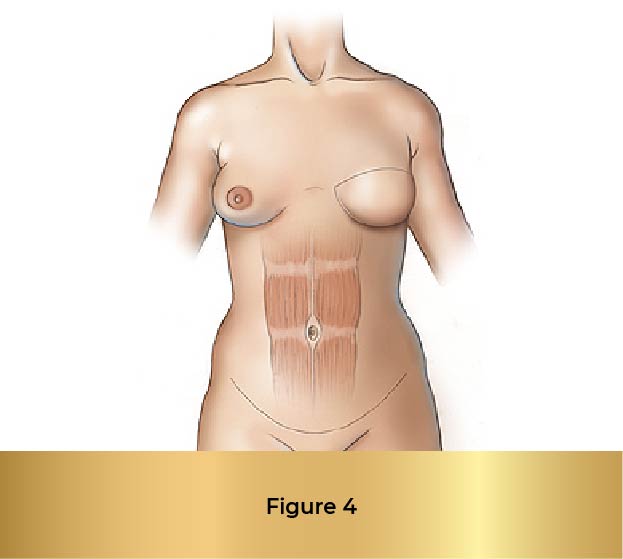
In the mid-1990’s it was recognized that the tissue used in a TRAM flap could be harvested without the rectus abdominis muscle by dissecting the blood vessels (the perforating vessels to the skin and fat) through the muscle (see figure 2). This flap, called the deep inferior epigastric perforator or DIEP flap (see figure 3), uses the same skin and fat of the lower abdomen as the TRAM to reconstruct a breast. There are several published series in the medical literature that show that patients who undergo this procedure have less pain and a faster recovery than patients who undergo TRAM flap reconstruction. There is also less risk of abdominal wall weakness and herniation. Finally, since the flap is taken from the low abdomen like a TRAM flap, there is the added benefit of a “tummy-tuck”, with the abdomen nicely re-contoured.
The DIEP harvest is longer and more complicated than a TRAM flap, but for most patients this is more than offset by the benefits to the abdominal wall.
Nearly every woman can opt for a DIEP reconstruction procedure, with the exception being women who lack enough abdominal fat tissue to create a breast. Younger women who are extremely athletic may fall into this category. In these patients, fat tissue can sometimes be harvested from other parts of the body, such as the inner thighs or gluteal areas, to reconstruct a breast.
In approximately 15% of patients, there are no large perforators coming through the muscle. In these patients the skin and fat of the lower abdomen are supplied by a more superficial blood vessel, the superficial inferior epigastric artery. This blood vessel is a branch of the femoral artery, and courses through the tissues of the lower abdomen without going through the rectus abdominis muscle. In these patients breast reconstruction can be performed with a flap of fat and skin from the lower abdomen without having to dissect through the rectus abdominis muscle. This flap is called the superficial inferior epigastric artery or SIEA flap.
Each time that Dr. Kind or Dr. Chang dissects a DIEP flap, he carefully looks for and preserves the superficial inferior epigastric blood vessels. If these vessels are of sufficient size, the SIEA flap can be used.
What About the Other Breast?
For women with breast cancer in one breast, the preoperative planning should always include a discussion regarding the opposite breast. Symmetry is one of the main goals of breast reconstruction. In many patients symmetry can best be accomplished by treating the opposite breast with augmentation, reduction or lifting. These procedures are covered by insurance, as mandated by law. In addition, significant breast asymmetry as a result of lumpectomy/radiation or multiple biopsies can be corrected with reconstructive surgery.





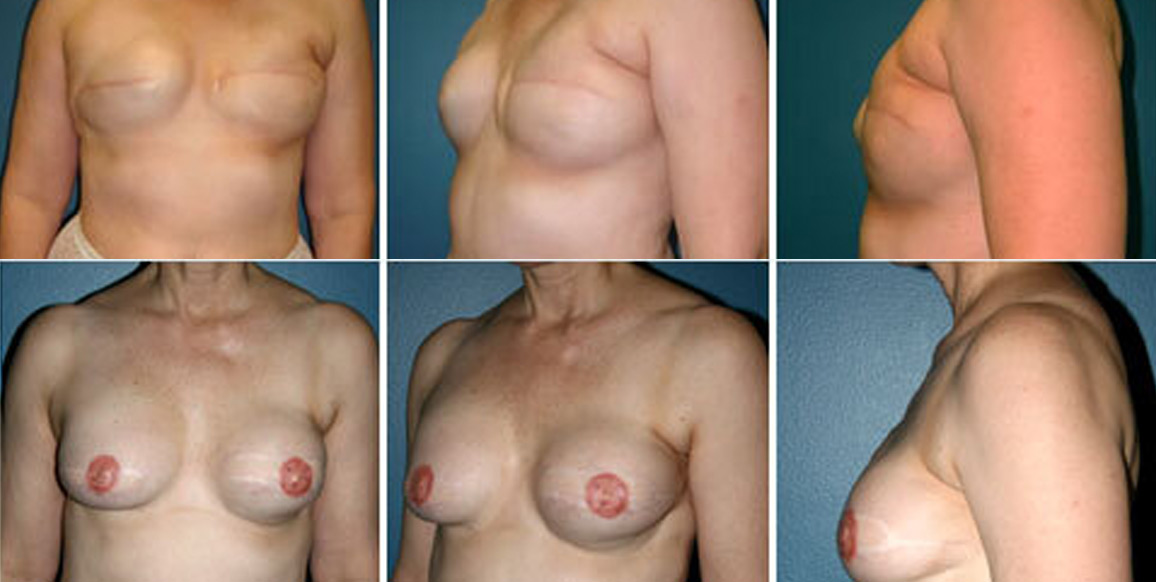
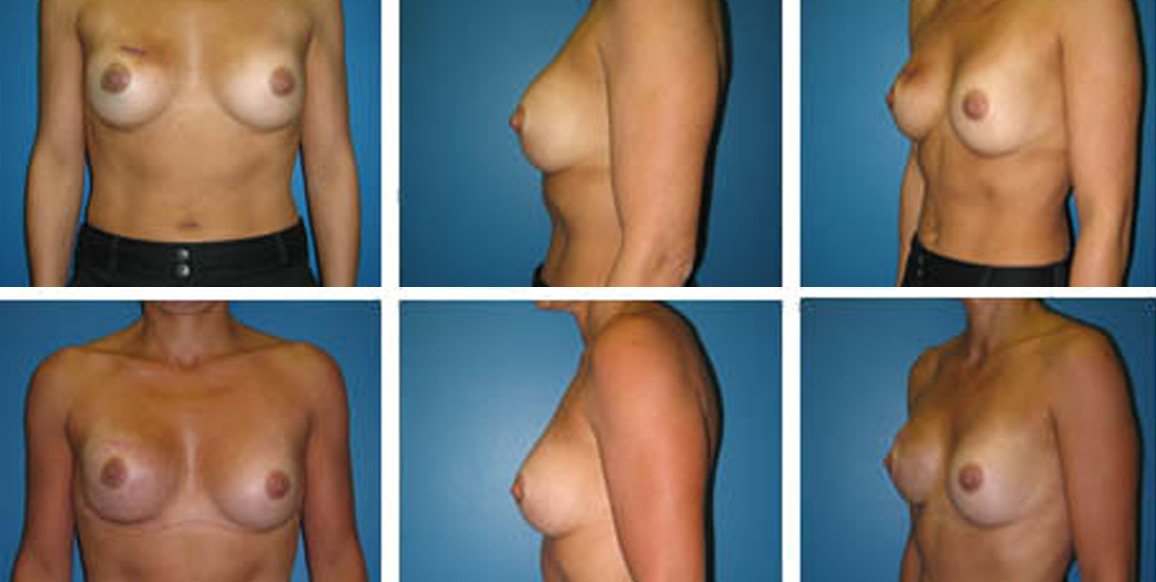


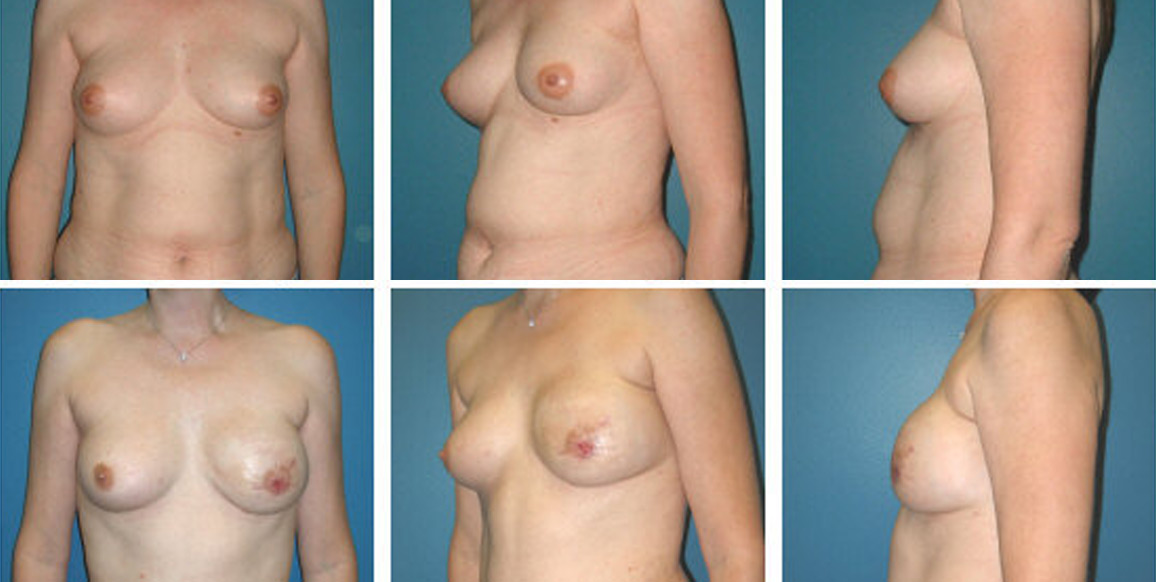


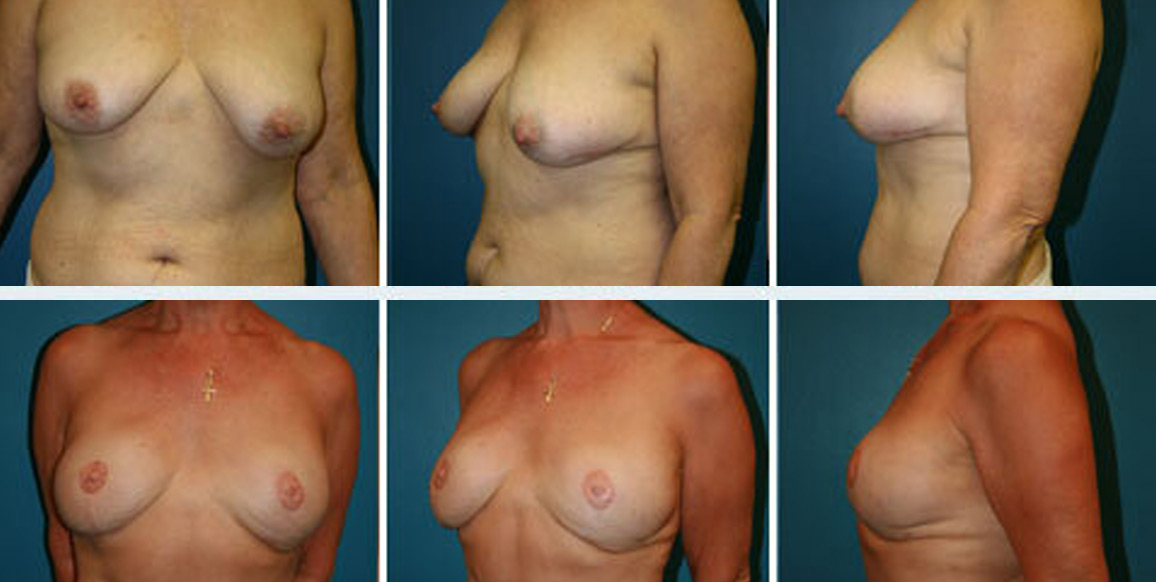
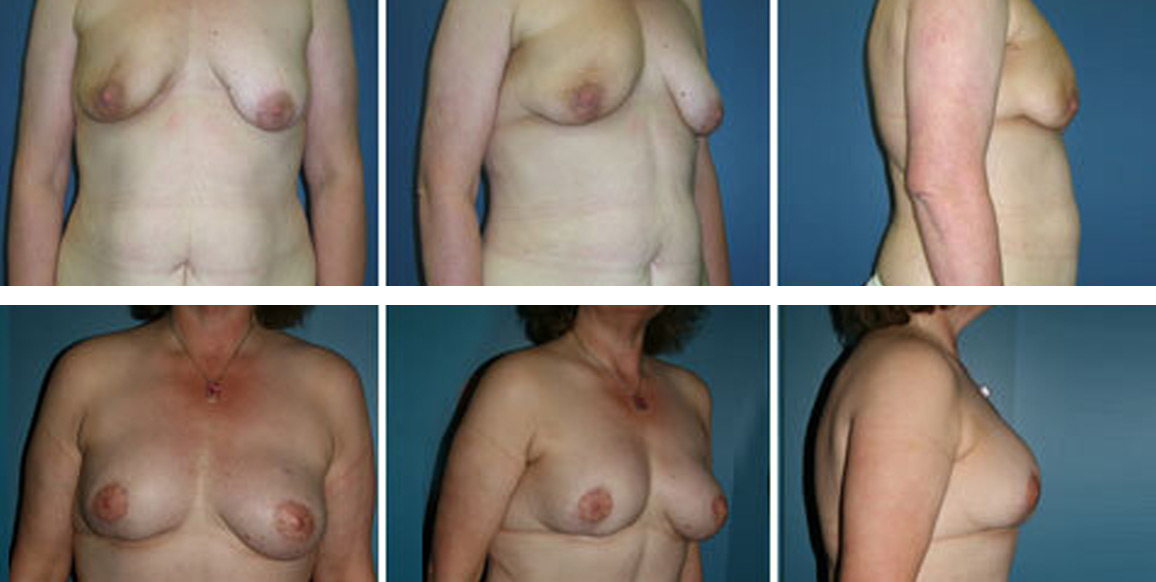
DISCLAIMER: Before and after results are NOT a guarantee that your results will be the same or similar. Each patient’s results will be different. Your results will vary from other patient’s results.
